New national reporting has once again highlighted how racism and discrimination remain powerful forces shaping health outcomes in the United States. In New England, these inequities persist despite the region’s reputation for advanced hospitals and medical research. Communities of color, immigrants, and low-income families across Massachusetts, Connecticut, Rhode Island, Maine, New Hampshire, and Vermont continue to face unequal access to care and poorer health outcomes.
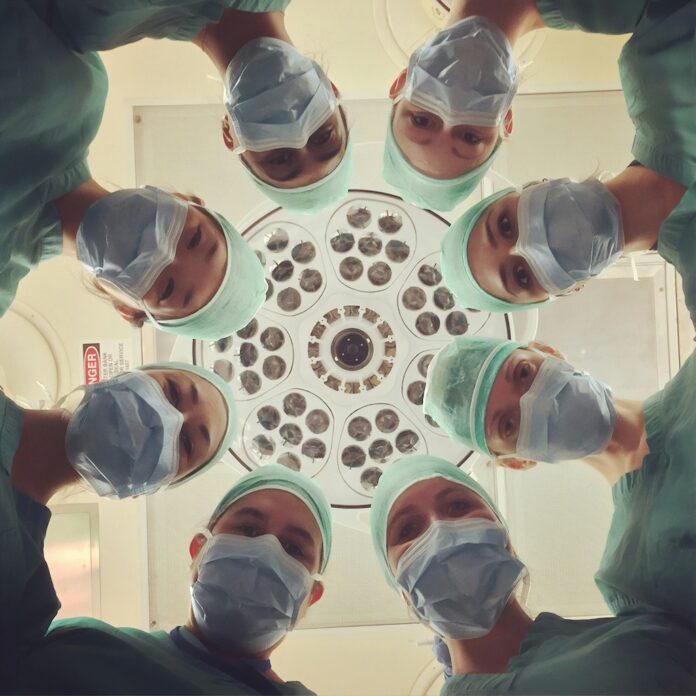
Bias and Unequal Treatment Inside Medical Settings
Across New England, patients of color report experiences that reflect long-standing patterns of bias in health care. These include having symptoms minimized, pain inadequately treated, or concerns dismissed altogether. National research shows that racial bias—often implicit rather than intentional—can influence clinical decision-making, leading to delayed diagnoses and worse outcomes for Black and immigrant patients. In cities such as Boston and Providence, advocates say these patterns contribute to deep mistrust between marginalized communities and health institutions.
Immigration Status and Fear as Barriers to Care
For immigrant families across New England, discrimination in health care is compounded by fear. Even when clinics are legally permitted to serve all patients, many immigrants hesitate to seek care due to concerns about immigration enforcement, data sharing, language barriers, or misunderstanding public benefit rules. In communities such as Lowell, Lewiston, and New Haven, this fear often results in delayed treatment for preventable or manageable conditions like diabetes, asthma, and high blood pressure.
Health disparities in New England cannot be separated from broader structural issues. Housing instability, food insecurity, environmental exposure, and low-wage employment all play a role in shaping health outcomes. Communities of color are more likely to live near highways, industrial areas, or older housing with environmental hazards, while many low-income workers lack paid sick leave or flexible schedules needed to attend medical appointments. Public health experts emphasize that these conditions—rooted in systemic inequality—translate directly into shorter life expectancy and higher rates of chronic illness.
Community Clinics and the Push for Health Equity
Community health centers across New England have become a critical safety net for uninsured and underinsured residents, offering culturally responsive care, interpretation services, and sliding-scale fees. While these clinics help reduce gaps in access, advocates warn they are increasingly strained by rising demand and limited funding. Health equity leaders argue that meaningful progress will require policy changes that address discrimination directly, expand coverage regardless of immigration status, and invest in prevention rather than crisis care alone.
Dr. Brian Omolo is an author and professional advisor dedicated to raising the voices of the different communities of New England. He is a PhD holder in Literature from Kenyatta University and a bachelor's degree holder in Pure Mathematics from the University of Nairobi, which justifies his combination of analytical clarity and creative insight.